Conditions
Trigeminal Neuralgia in Singapore
Overview
What is Trigeminal Neuralgia? What are the Types of Trigeminal Neuralgia? What Causes Trigeminal Neuralgia? Signs and Symptoms of Trigeminal Neuralgia Risk Factors for Trigeminal Neuralgia How is Trigeminal Neuralgia Diagnosed? How is Trigeminal Neuralgia Treated? Can Trigeminal Neuralgia Be Prevented? When to Seek Medical Attention for Trigeminal Neuralgia?

Dr Thor Timothy
Consultant Pain Specialist & Anaesthesiologist
MBBS (S'pore), MMed (Anaesthesiology), FFPMANZCA (ANZCA, Australia/New Zealand), EDPM (Europe),FAM (S'pore)
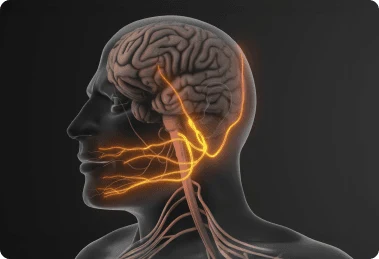
What Is Trigeminal Neuralgia?
Trigeminal neuralgia (TN) is a chronic pain condition affecting the trigeminal nerve, which is responsible for transmitting sensation from the face to the brain. It is characterized by sudden, severe, and often debilitating facial pain. The pain is typically triggered by everyday activities such as talking, chewing, or even a light touch. Trigeminal neuralgia is considered a very severe pain disorder that significantly impacts a person’s quality of life.
What Are the Types Of Trigeminal Neuralgia?
Trigeminal neuralgia is classified into different types based on the nature and severity of symptoms:
Type 1 (Classic or Typical Trigeminal Neuralgia) – Characterized by sharp, electric shock-like pain episodes that come and go. These attacks last from a few seconds to minutes and can occur in cycles over weeks or months.
Type 2 (Atypical Trigeminal Neuralgia) – Involves constant, aching, burning, or stabbing pain in addition to the intermittent sharp attacks. This type is often more difficult to treat.
Secondary Trigeminal Neuralgia – Caused by an underlying medical condition, such as multiple sclerosis or a tumor compressing the trigeminal nerve.
What Causes Trigeminal Neuralgia?
The primary cause of trigeminal neuralgia is the compression of the trigeminal nerve, often by a blood vessel pressing against it. Other possible causes include:
Ageing – Structural changes in the nerve and surrounding blood vessels over time.
Multiple Sclerosis (MS) – Damage to the protective nerve covering (myelin sheath) can result in TN symptoms.
Tumors or Cysts – Growths pressing on the trigeminal nerve can trigger pain episodes.
Facial Trauma or Surgery – Injury or surgical procedures involving the face may damage the nerve.
Arteriovenous Malformation (AVM) – Abnormal blood vessel formation can compress the nerve.
Idiopathic Cases – In some instances, no clear cause can be identified.
Signs And Symptoms Of Trigeminal Neuralgia

Trigeminal neuralgia is characterized by the following symptoms:
Sudden, intense, electric shock-like pain in the face
Pain affecting one side of the face, typically along the jaw, cheek, or eye
Episodes lasting from a few seconds to minutes
Recurring pain attacks triggered by activities like talking, chewing, brushing teeth, or touching the face
Periods of remission where no pain is felt, followed by recurrences
In atypical cases, a persistent burning or aching sensation between attacks
Pain intensity increasing over time if left untreated
Risk Factors For Trigeminal Neuralgia
Several factors increase the likelihood of developing trigeminal neuralgia:
Age – More common in people over 50
Gender – Women are more likely to develop trigeminal neuralgia than men
Family History – Genetic predisposition may play a role in some cases
Neurological Disorders – Conditions like multiple sclerosis increase the risk
High Blood Pressure – Increased vascular pressure may contribute to nerve compression
Facial Trauma or Surgery – Previous injuries may damage the nerve


How Is Trigeminal Neuralgia Diagnosed?
A pain specialist will use various methods to diagnose trigeminal neuralgia, including:
Medical History and Symptom Evaluation – Reviewing the patient’s pain patterns and triggers.
Physical and Neurological Examination – Assessing facial sensitivity and nerve function.
Magnetic Resonance Imaging (MRI) – Identifying nerve compression, tumors, or multiple sclerosis.
Trigeminal Reflex Testing – Evaluating the function of the trigeminal nerve.
Trigeminal Neuralgia Singapore: Treatment & Specialist | Dr Thor
The treatment approach depends on the severity of the condition. Options include:
Medications
Anticonvulsants (e.g., carbamazepine, oxcarbazepine) – Help stabilize nerve activity and reduce pain episodes.
Muscle Relaxants (e.g., baclofen) – May be used in combination with anticonvulsants.
Tricyclic Antidepressants (e.g., amitriptyline) – Sometimes prescribed for atypical trigeminal neuralgia.


Can Trigeminal Neuralgia Be Prevented?
There is no guaranteed way to prevent trigeminal neuralgia, but certain lifestyle habits may reduce the risk or minimize flare-ups:
Managing blood pressure to reduce vascular compression.
Avoiding known triggers such as cold air, chewing hard foods, or facial pressure.
Reducing stress, as anxiety and tension can exacerbate symptoms.
Maintaining good dental hygiene, as dental infections may contribute to facial nerve irritation.
When To Seek Medical Attention For Trigeminal Neuralgia?
Seek medical care if you experience:
Severe, recurring facial pain that interferes with daily life
Pain that worsens over time or becomes unresponsive to medications
Numbness, weakness, or tingling in the face
Symptoms associated with multiple sclerosis, such as vision problems or muscle weakness
Side effects from medication that impact quality of life

GET IN TOUCH
Contact Us Today
For more information about our services, or to make an appointment, please reach out to us. We will get back to you as soon as possible.

Frequently Asked Questions
No, stress does not cause trigeminal neuralgia, but it can worsen symptoms by increasing muscle tension and sensitivity. Stress management techniques may help reduce flare-ups.

Trigeminal Neuralgia Pain Specialist in Singapore
Dr Thor Timothy
Consultant Pain Specialist & Anaesthesiologist
MBBS (S’pore), MMed (Anaesthesiology), FFPMANZCA (ANZCA, Australia/New Zealand), FIPP (USA), EDPM (Europe), FAM (S’pore)
MBBS (S’pore), MMed (Anaesthesiology), FFPMANZCA (ANZCA, Australia/New Zealand), FIPP (USA), EDPM (Europe), FAM (S’pore)
Accreditations & Qualifications:
Bachelor of Medicine, Bachelor of Surgery (Singapore)
Master of Medicine in Anaesthesiology (Singapore)
Fellow of the Faculty of Pain Medicine, Australian & New Zealand College of Anaesthetists
Fellow of Interventional Pain Practice (USA)
European Diploma in Pain Medicine
Fellow of the Academy of Medicine, Singapore
Dr Thor Timothy is a consultant anaesthesiologist and pain specialist in Singapore with nearly 20 years of medical experience, including over a decade in pain medicine. Formerly the Director of Acute Pain Services at Singapore General Hospital, he has a special interest in trigeminal neuralgia treatment and management of other chronic facial pain conditions. He provides personalised, minimally invasive treatments to help patients find relief from nerve pain and improve their overall well-being. He holds multiple international pain medicine qualifications and is dedicated to delivering compassionate, multidisciplinary care tailored to each patient’s needs.
